 |
| Image Source http://www.viartis.net |
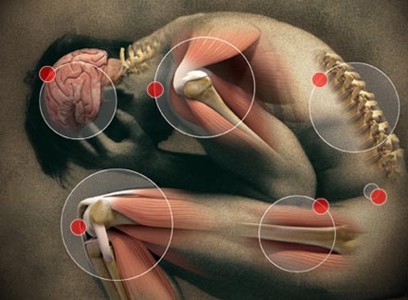
Parkinson’s disease was believed to be a, motor debilitating disease mainly dealing with loss of dopaminergic neurons in the substantial Nigra[1]. However recent developments have shown that Parkinson’s disease seems to have an effect on other regions of the brain, associated with non-motor control[1]. These symptoms can often times precede the onset of motor related symptoms by up to 10 years[2]. Characteristic pre-motor symptoms include: Sleep Disorder based symptoms, Autonomous Dysfunction symptoms and Neuropsychological symptoms[3]. These symptoms can also occur in comorbid manner, to the extent that the establishment of one symptom leads to the occurrence of another symptom, this is particularly implicit in both sleeping disorders and neuropsychological disorders[3]. Current studies have shown that both sleep disorder and autonomous dysfunction may play an integral role as neurological markers for the potential development of Parkinson’s disease. This, researchers believe could be vital in the development and implementation of psychoactive drug or Deep-Brain Stimulation treatments to target the disease in its earliest state[4].A definite hypothesis on the causes of these symptoms is still unknown; however multiple studies have depicted the notion of dopamine deficiency in different regions of the brain as the inherent cause of these non-motor symptoms[4].
|
Table of Contents
|
[— Place your main content below. —]
1 Sleep Disturbances
1.1 Signs and Symptoms
Sleep disorders are implicated in 90% of patients and often times the first signs of a person developing the disorder[5]. Sleeping dysfunction in patients with Parkinson’s disease occurs in many forms including: Rapid eye movement disorder REM , insomnia including nocturia, impaired day time alertness, and Restless leg disorder. Rapid eye movement disorder is one of the most common forms of sleep disorders associated with Parkinson patients, specific importance as a crucial early detection marker for detection of Parkinson[5]. The characteristic signs of REM disorder are the development of vivid dreams being acted out through motor movements, mainly as a result of the lack of paralysis associated with being in the REM[2]. The loss of this motor related paralysis during REM sleep occurs due to a decline or degeneration of muscle Antonia that works in inducing this paralytic state[2].
Insomnia is another highly prevalent sleep dysfunction symptom estimated to affect 90% of all Parkinson’s patients[2]. It is often a very destabilizing disease and is responsible for majority of the intense suffering patient’s undergo[2]. Insomnia occurs in several different forms including: nocturia which is frequent visits to the washroom at nights, dysfunctional breathing during sleep, intense pain and night time tremors[2].
Impaired daytime alertness also known as EDS (Excessive daytime somnolence) is estimated to affect approximately half of the total number of Parkinson patients[2]. EDS is characterized by tiredness, lack of energy and intense urge to fall asleep spontaneously[3]. An extreme form of impaired daytime alertness symptom is known as sleep attack; which is a sudden induction of sleep[2]. Many studies have shown that sleep attack is prevalent in up to 43% of Parkinson’s patient[2]. The everyday activities of a patient with Parkinson’s disease can be affected by the destabilizing nature of sleep attacks and EDS3. Specifically; damage can be caused during activities such as operating motor vehicles or being at work.
 |
| Figure is a proposed model for the dysregulation of circadian cycle. Image Source Videnovic and Golombek, 2012 |
1.2 Early Detection and Potential Causes of Sleep Disorders
Early detection of sleep disorder in Parkinson’s patients is an interesting but integral factor in early diagnosis of Parkinson’s disease. Multiple studies have shown that sleep disorder symptoms specifically Rapid Eye movements may precede the onset of motor related symptoms by decades depending on individual[5]. These early sleep disorder symptoms may be due to steady loss of dopaminergic neurons in the Suprachiasmatic nucleus (SCN); a small region in the brain that has been identified to be involved in the Circadian Rhythms[2]. The circadian rhythm in mammals specifically humans, is a endogenous cycle that controls multiple processes and central in maintaining the sleeping and alertness cycle[6]. As such a decline in dopamine leads to a disruption of this cycle and eventually to the development multiple sleep disorder symptoms[3]. This process however maybe reversible or prevented with the use of psychoactive drugs used to increase dopamine level in suprachiasmatic nuclei region of the brain[2]. By doing so during early periods of the illness it may be possible to halt the decline of dopamine in the brain[4].
2 Autonomous Dysfunction
There are two categories of autonomous dysfunction namely; major symptoms ad minor symptoms. The major symptoms include: Sympathetic cardiac denervation and orthostatic hypotension[4]. Minor symptoms include: erectile dysfunction, nycturia, gastrointestinal disorder, constipation, dysphagia, seborrhea and urinary retention[7].
2.1 Major Symptoms
Loss of sympathetic cardiac innervation otherwise known as sympatric denervation is a nuero-circulatory dysfunction that involves a substantial but progressive decrease in the heart rate due to dramatic loss of functional cardiac nerve fibers[7]. Orthostatic hypotension is a symptom that affects approximately upwards of 40% between the ages of 25-65 of Parkinson’s patients; it is often associated with tiredness, feeling lightheaded or weak, dizziness and extremely low blood pressure, often leading to loss of cognitive function and in extreme cases death in older patients[8]. Orthostatic hypotension can be caused by either loss of cardiac nerves resulting from sympathetic cardiac denervation, byroflex failures or in some cases due to Levodopa treatmen[8]t. Levodopa is a psychoactive drug commonly associated with Parkinson’s treatment; it is used to increase the dopamine levels in specific brain regions[8]. However some clinicians believe it may be indirectly affecting other regions leading to development or exacerbation of different non-motor symptoms including autonomous dysfunctions[8].
2.2 Minor Symptoms
Minor symptoms of autonomous dysfunctions include two main groups: those with urogenital disorders including; erectile dysfunction, nycturia, and those with gastrointestinal symptoms; such as constipation, dysphagia and sialorrhea[9]. Erectile dysfunction and constipation are believed to be influenced solely by age[9].
Minor symptoms of autonomous dysfunction are generally more common but less detrimental to individuals with Parkinson’s disease[9]. On average these symptoms tend to occur between 28-57 percent of all Parkinson’s patient depending on the type of symptom, although some studies have shown the numbers to be slightly higher or lower[9]. Some of these symptoms for example sialorrhea and constipation tend to be intertwined with the specific stage of the illness, as such these symptoms may occur at later stages of the disease as oppose to major symptoms which are more early sign symptoms[9]. Evidence has also been produced to depict a commonality between Levodopa dosage and development of less severe autonomous dysfunction[9].
Dopamine receptors have been implicated in the development of both major and minor forms of autonomous dysfunction, for example a lack of regulation of the D1 receptors found in the micturition region of the pons has been suspected to be involved in urinary retention disorder[11]. This leads to an inability to control the detrusor muscle activity thus leading to the disorder[11].
2.3 Early Detection and Potential Causes
An integral aspect of autonomous dysfunction is the notion that Early detection may lead to proper diagnosis of Parkinson’s disease before any motor symptoms occurs. A case study by Goldstein et.al shows slight symptoms of autonomous system failures including sympathetic denervation and baroreflex-cardiovagal hypo-function occurring 4 years before any development of motor impairment[4]. The central cause of these early symptoms have been speculated to occur as a result of steady decline in neurotransmitters in the different brain regions, for example a decrease in Norephinephrine in the cardiac leads to loss of cardiac nerves cells several years, often times more than 4 years before any movement related problems occur[4].Early detection is just as essential in autonomous dysfunction symptoms as it is in sleep disorder symptoms. It works as an integral marker that may identify early signs of Parkinson's disease and lead to development and administration of essential drugs like levodopa during early stages of the disease, where it may have more effects as oppose to later stages where the substantial nigra loss may be to overwhelming[4].
3 Neuropsychological symptoms
3.1 Common Symptoms
Neuropsychology is a well-researched and constantly growing field in the study of Parkinson symptoms, specifically in the last couple of years. Psychosis symptoms of Parkinson’s are said to be prevalent in upwards of 25-50% of Parkinson patients[3]. These symptoms often range from minor to mild symptoms and are usually not very detrimental to the livelihood of the Parkinson’s patient; in comparison to other Parkinson related symptoms[3]. General nuerodegeneration symptoms of Parkinson’s include: Visual and auditory Hallucinations, dementia,and cognitive deficits[3].
3.1A Hallucinations and Delusions
Visual hallucinations: It is characterized as one of the most common forms of hallucinations in Parkinson’s patients affecting approximately 40% of individuals with Parkinson's disease[10]. Visual hallucinations occur in different forms in accordance to the severity, benign hallucination for example is a minor form that includes slight disorientation of consciousness but with near to perfect memory in tact[11].Other forms of visual hallucinations include Presence hallucination; in which an individual feels the presence of another organism (mainly person or animal), passage hallucination: whereby a patient begins to see or perceive a person or animal passing by their visual field[12]. Those two forms of hallucination fall under the category of Minor hallucinations that affect approximately 40% of patienst[12].
Auditory and tactile hallucination: Less prevalent forms of hallucinations being present in only 7-13% of patient, who also experience visual hallucinations[13]. Auditory hallucinations are characterized by perceiving whispers or small tones, but may become as scary as hearing confrontational voices[14]. Tactile hallucinations involve feeling of small creatures crawling along ones bodies’ [3].
The main causes of these Hallucinations have been widely speculated to be due to cognitive deficits Boyed by dysfunction of dopamine receptors in both the stratum and prefrontal cortex[2]. This leads to a loss attention or working memory which ultimately contributes to a lack of control over which visual or auditory stimuli/information to focus on and which to discard and thus leads to hallucinations[15]. In addition lack of dopamine regulation in the prefrontal cortex to basal ganglia interaction has also been implicated in contributing to the issue[15].
Delusions: A prevalent symptom in Parkinson patients said to influence 8% of the overall Parkinson patients [16]. Delusions occur in many different forms including: grandiose (feeling of superiority), paranoia, somatic (feeling of things crawling through your body), persecutory etc[17]. The most interesting aspect of delusions is the fact that they occur in younger patients as opposed to hallucinations that occur mostly in older populations[18].The causes of delusions are often times attributed to the same pathways of those that caused hallucinations in patients[11]. In addition acetyl choline has also been speculated to have an impact in causing dementia related symptoms due to partial successes observed in Parkinson patients given ACHL psychoactive drugs[2].
3.1B Cognitive Deficits and Mood Disorders
Depression: Is often times characterized as the most prevalent psychotic disorder in Parkinson patients, affecting approx72% of patients in the first couple years of diagnosis[18]. Depression occurs in different forms raging from mild to severe, and symptoms of it can be perceived even before any motor impairment signs occur[2]. Depression is associated with a multitude of symptoms that affect day to day life including; cognitive dysfunction, apathy, tiredness, lack of sleep[2]. Causes of depression in Parkinson patients have been speculated to involve dopamine dysfunction in different regions of the brain[2].
Dementia is a cognitive deficit disorder affecting approximately 40-80 percent of Parkinson patient if properly diagnosed[2]. Dementia has often been thought of as a late occurring symptom due to many physicians inability to recognize the signs early on, as oppose to other symptoms like tremors which are often more recognizable[2]. Common signs of dementia include; impairments in cognition, emotional regulation, memory, and attention. These cognitive deficits occur as a result of Deterioration of neurons in different regions of the frontal and temporal lobe for example the amygdala and ventromedial lobe[2].
| Example heading |
| Jo Collinge explains some of the common non motor symptoms of Parkinsons, their effects and why early detection is integral. |
3.2 Comorbidity
An intrinsic aspect of the neuropsychological symptom however, is the fact that it is mainly prevalent in a comorbid manner with other non-motor symptoms[19]. In fact some of the main causes of these symptoms are said to be due to other non-motor factors, most common symptoms attributed to causing nueropsychiatric disorders is REM sleep disorder and dementia[19]. A study by Lee.et.al presented multiple evidences indicating that Parkinson patients with sleep or mood disorders were five times more likely to develop psychotic symptoms; In addition the paper depicts a strong association between the development of dementia and psychosis[19]. Other studies have theorized the occurrences of one symptom to be as a result of comorbidity, One such study depicted the occurrence of hallucination correlated with dysfunctional sleep disorders[19]. A study by Mokoswitz In support of his continuum hypothesises, concluded that 61% of hallucinations occurred due to REM disorder like symptoms[11].


This Neurowiki is quite interesting! Would this article "Epigenetics in Parkinson's and Alzheimer's diseases." on the epigenetics of parkinson's and alzheimer's help in expanding your co-morbidity subtopic?
yup i think it would
I look forward to linking up your wiki page with mine! A lot of the symptoms (eg. motor and visual) I also discuss in my wiki but I tend to focus more on task-dependent outcomes. It's really interesting to learn more about the clinical symptoms!
Like I mentioned before, I really like your topic because a lot of people tend to forget about the non-motor symptoms. I would change the title of your individual page though to indicate that you will mainly discuss the non-motor symptoms.
This may also be a problem on my end but I can't seem to see some of your images (the 2 in the body). It may also be a good idea to organize what's under 1.3a into their own subheadings.
Are you planning to discuss any of the medical side-effects that may also present themselves in a PD patient?
Good work!
That is true thank you very much, I should/am going to change the title non-motor symptoms seems more fitting.
also very good points for the 1.3a part, i was thinking of doing it before but yeah Ill do that too.
Umm on your last point i tended to focus mainly on these non-motor symptoms and only barely mentioned side effects caused by drugs like levodopa so nah, I am only focusing on the symptoms as a sole entity as oppose to getting into the sides effects aspects.
Thank you for your output it was really helpful.
Hey Igbi :D Sorry for being so late in your wiki.
This looks like a great summary of all the non-motor PD symptoms that many don't usually know about.
I feel like sometimes people just think PD is all about the motor symptoms, but after researching and reading your wiki I can tell there is much more to it.
For my section, I also have a little section on PD dementia so I will link it to yours.
Also I just saw some "buggy coding" — I think you should delete the "[-Place your main content below-]". And under 3.1B, you wrote "Depression: Is often times characterized…". I think it would look better if you just took the colon.
All in all, great work!
Read through your page completely and I really enjoy your writing style Iggy.
You definitely put a lot of effort into this and the page looks great!
Side Note: "Example Heading" is still on top of your video :P Also, I'm not sure if this is correct, but when you mention a research group like Goldstein et al….shouldn't you include the year after it. (i.e. Golstein et al. (year)…..)????
All in all this is put together very well and it flows really well too.