| Cochlear Implants |
 |
| "Hey, listen" Image Source: Gizmodo[5] |
According to the World Federation of the Deaf there are 70 million deaf individuals around the world.[1] Life for the hearing impaired has greatly improved over the decades with great headway made in the advances of cochlear implants (CI). At this current time, the success of cochlear implants is variable and despite best efforts they are not perfect. One of the biggest debates regarding cochlear implants is confirming whether or not the procedure is worthwhile to specific populations. Various studies conclude the success of the implants is largely age-dependant.[2] Closely linked with age is a candidate’s level of language acquisition prior to hearing loss.[3] Those afflicted with deafness prior to language acquisition are significantly hindered compared to those who have learned language. Deprivation of verbal language alters neurological structures which consequently result in prelingual cochlear implant users having a harder time rehabilitating.[4] This prelingual caveat can be bypassed to some degree if the cochlear implant is implanted before the critical window of development closes.
Partaking in preoperative research and committing to the surgery is only half the journey for cochlear implant candidates. Once the implant has been surgically placed into the body, patients must to adjust to their new device and way of life. Children tend to benefit more from the implants than adults do, and postlingual recipients learn faster than prelingual recipients.[3] [4] Despite its limitations, most recipients of cochlear implants report satisfaction with their devices. Apart from the restorative ability of cochlear implants, implants have provided its users with psychological benefits such as autonomy and social inclusivity.
|
Table of Contents
|
Premises for Rehabilitating Prelingually Deaf Children with Cochlear Implants
OVER-ARCHING GOALS
- Learn to associate meaning to CI transferred sounds.
- Communicative competence is the ultimate goal of rehabilitation.
LEARNING ENVIRONMENT
- Learned skills need to be transferrable settings outside of therapy. i.e. school, home, daycare
- New skills need to be integrated into appropriate social and emotional contexts.
- Parental support can greatly influence how well a child adapts to their CI
CONTENT AND EXPERIENCE
- Acquisition of spoken language requires a combination of didactic instruction and incidental learning.
- Diagnostic teaching provides the most benefits as it acknowledges the limits of a child’s ability.
- Integrating school work into the rehabilitation curriculum will maximize learning efficiency.
- Music can be used as learning tool because of its ability to evoke complex auditory experiences.
- Infants and toddlers require different learning approaches than children.
MONITORING PROGRESS
- Individual auditory milestones should be generated for each child.
- Formal assessment tools can provide a general evaluation but they do not provide a comprehensiveness assessment of language skills.
Guideline adapted from:
Chapter 12 of Cochlear Implants:
Principles & Practices[21]
1.1 A Brief History
| First in 1978 |
 |
| Rod Saunders (right) first successful CI recipient Image Source: SMH[10] |
See also: Interactive Timeline
1957: First clinical cochlear implant (CI) attempted by Djourno and Eyriès.[6]
1961: Short-term CI clinical trials begin on adults.[7]
1972: Dr.William F. House's 3M single-electrode implant is the first to be commercially marketed.[7]
1978: Rod Saunders becomes the first recipient of an Australian implant, invented by a team led by Dr. Graeme Clark.[8]
1984: Cochlear implants are approved by the United States FDA for adults.[8]
1985: Clinical trials for CI in children begin. Bryn Davies (5yrs) and Scott Smith (10yrs) become the first pediatric recipients.[8]
1990: The FDA allows CI for children as young as two years of age.[9]
2000: The FDA lowers the age restriction to 12 months.[9]
In less than 30 years after the first successful implant, thousands of deaf and hard-of-hearing people have regained their ability to hear. As of December 2010, the U.S. Food and Drug Administration (FDA), estimates that 219,000 people around the world have received a CI. Roughly a third of those recipients reside in the United States; 42,600 whom are adults and 28,400 whom are children.[9]
2.1 Rehabilitation
| Enhanced Visual Processing Demonstration by Double Dissociation |
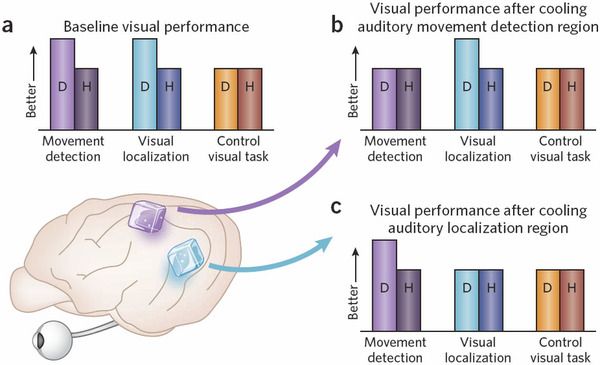 |
| Fig. 1 a) Under normal conditions, deaf cats excel in supramodal tasks; D, deaf cats; H, hearing cats. (b)(c) Hindering one area of the brain selectively decreases performance detection in D cats. The take away message is the enhanced abilities D cats show in supramodal tasks.[20] |
See: Right Side Bar
2.1a Brain Plasticity
See also: ‘Unused’ Auditory Cortex
Brain plasticity is one of the major obstacles in rehabilitation after cochlear implant surgery. Particularly true in those who are prelingually deaf, the brain maximizes itself by allowing the visual system to take over its silent auditory cortex. This phenomenon is known as cross-modal plasticity, and it changes brain circuitry to allow active sensory modalities to compensate for the deprived cortex.[11][12] Due to the integration of the visual system, some CI recipients may benefit from rehabilitating strategies that associate sounds with visual cues.[11][13] With sufficient practice and sensory stimulation, even adult brains can be rehabilitated.[14]
2.1b Language Acquisition
As early as in utero, the auditory system of a fetus can be stimulated by environmental sounds. Many mothers who speak or sing to their unborn child will anecdotally agree that their child can respond to the sound of their voice. A fetus can react to sound stimuli as early as 38 weeks into gestation as discovered by DeCasper and colleagues.[16] Not only can the child detect sound, they are also able to differentiate between familiar and novel stimuli which is reflected in their heart rates.[16] This occurrence suggests infants can code ambient language before they are even born through process such as pattern detection. Developing the mechanisms for language acquisition is crucial within the fetal, neonatal, and infant stages of life. The importance of early detection for deafness and intervention is stressed even more so because of these findings.
For people with cochlear implants, learning verbal language after surgery will be like learning a second language. This phenomenon has been recognized as late first language acquisition, and alters the functional and structural organization of the brain.[17] Since sign language heavily utilizes the motion-sensitive visual cortex, language acquisition of spoken language will require extensive new learning techniques that differ from previous processes.[18]
Four interrelated systems of language development[19]
- Pragmatic Development
- Phonologic Development
- Semantic Development
- Grammatical Development
 |
| Superior Temporal Gyrus Image Source: BodyParts3D[15] |
2.1c Superior temporal gyrus
See also: Brain Regions Activated in Language Processing
The Superior temporal gyrus (STG) contains the primary auditory cortex, which is associated with speech production and auditory processing. The Brodmann areas and Wernicke’s areas, regions responsible for language processing are also located within the STG.[13] In deaf subjects, these areas are underdeveloped (See brain plasticity). After the introduction of CI, some patients can redevelop their STG to associate with sound and language. However this is not always the case as found by Giraud and colleagues; their results indicated neural development can occur around the STG instead than within the region.[22] Using positron emission tomography (PET), CI users activated novel non-auditory regions, such as the dorsal occipital cortex, when presented with words, syllables and environmental sounds.[22] These findings indicate that functional specificity in deaf brains and those who regain hearing develop differently than those of hearing.
2.1d Never Too Late
Many cochlear implant recipients will remember the first sound they hear after surgery, and the experience of it is an emotional one. Opting in for a CI is a life changing process that can benefit patients of all ages. It is never too late to consider oneself for the implantation (see video: “Hearing for the First Time”).
In Fig. 2, all participants of the study were over the age of 50 years old and the mean age of implantation was 63.4 years. While brain plasticity in children are more malleable than adult’s, results indicate elders can still benefit from CIs.[14][23] Improvement in speech perception is seen in adults as old as 80 years of age.[24] If adults are considering CIs, assessing the risks, seeking preoperative counseling, and having realistic expectations will garner the most satisfactory results.[25]
| “Hearing for the First Time” |
| Sarah Churman hears her own voice for the first time with the help of the Esteem cochlear implant by Envoy Medical. |
2.2 Implants on Different Populations
2.2a Prelingual vs. Postlingual Deafness
| "Speech Performance in Older Adults" |
 |
| Fig. 2 Mean CID sentence scores obtained in subjects with postlingual hearing impairment just prior to cochlear implant surgery and at 6 and 12 months.[24] |
Prelingual deafness is the onset of hearing loss before the age of language acquisition. In research, children diagnosed with deafness prior to 2 years of age are generally considered prelingually deaf.[26] A more stringent prelingual age cap also defines impairment at 12 months or less as a marker. [27][28] Since developmental milestones differ from child to child, brain structure alterations that result from deficient verbal communication is probably the best distinction between those who are prelingually and postlingually deaf.[27]
Postlingual deafness is classified as late onset hearing loss where partial or full language acquisition has been achieved. People who are considered postlingually deaf develop some cortical structures for verbal and auditory processing before hearing is lost. Since neurons for language have been partially developed, postlingual patients tend to benefit more from cochlear implants. Statistically, children with postlingual hearing loss adapt to CIs faster than prelingually deaf children.[27] While prelinguals children require 24 months to show improvement in speech perception, postlingual children demonstrated new skills after 6 months.[29] At 36 months, the performance scores between the two groups are reduced and become relatively equal.[29] The disparity between the two groups in the early months of CI suggests the importance of prior learning. The delayed improvement demonstrated by the prelinguals reveals that brain plasticity can still influence learning even after critical windows of development.[29]
2.2b Children vs. Adults
See also: Assessment of Candidacy: Age
As brain plasticity is considered the major limiting factor in CI success, delaying the implant even by several months can significantly hinder later language learning. When language skills of CI children were assessed (e.g. receptive and expressive vocabulary, verbal intelligence, and receptive and expressive language), children who received implants earlier in age consistently did better than those with later implants.[30] The question arises of whether CIs are appropriate for adolescents and older adults who have past the advantageous 12 month window.
Young CI patients have the opportunity to catch up with their hearing peers if the surgery is done early. Previously deaf CI adults do not have the ability and plasticity to perfect their perceptual skills, but CIs do help elders significantly improve their quality of life. Emotional health is one of the largest improvements.[24] A questionnaire by Horn et al. found comparable rates of quality of life benefit (87%), increased social activity (57.4%), and increased confidence (80.9%) for older cohorts.[31]
3.1 Psychological Implications
3.1a Quality of Life & Self-Esteem
| "Parameters of Self-Esteem: Deaf vs. Hearing" |
 |
| Fig. 3 Parental ratings on various parameters of self-esteem for normal hearing (NH) and cochlear implant (CI) children. Only one significant difference was found, which was in level of activity.[35] |
Objective and subjective studies of CI recipients report increased levels of satisfaction in life after the implants. Quality of life (QoL) measures the general well-being of an individual.
An assessment of children (aged 4-7) revealed that subjective assessments of QoL for children with CIs are not significantly different from that of their hearing peers.[32] Parents and teachers have also reported the successfulness of cochlear implants through observation inside and outside the classroom environment. When contrasted with the normal hearing, children with CIs are rated just as happy, confident and independent (see Fig. 3). Higher levels of self competence help children to develop a sense of independence. Overall, research confirms that CIs have the potential to produce positive changes a in child’s academic and family life. Positive subjective and objective observation are reported regardless of improvement in skill.[33] Children are able to provide researchers with more personal data, but it should be noted that their overall ratings of QoL (cognitive, emotional, and social development) tended to be higher than that of their parents.[32] Despite the disparity, both parent and child’s assessments generally complement each others in a positive light.
Increase of self-esteem is high among adolescents with cochlear implants. The improved self-esteem is in part due to group inclusion, which can be aided by acquired hearing. People feel more satisfied with life when they perceive a sense of closeness with their friends and classmates. [34] Self-esteem and social-well being is similar and at times even better than normal hearing peers.[35] In older adults, hearing provides a sense of mastery and autonomy that bolsters also self esteem.[24]
4.1 Ethical Complications
| "A Bionic Kid" |
 |
| Aiden K. got two cochlear implants when he was 10 months old to deliver signals to his auditory nerves. Image Source: Mark Thiessen, National Geographic[41] |
The progressive field of cochlear implants has exploded over the last few decades, providing thousands with renewed hearing, but like many practices, it is not without ethical controversies. Since the first implant in 1978, the FDA has been approving CIs for increasingly younger candidates.[9] While children as young as 12 months are eligible for a CI, infants such as Aiden K. (see image “A Bionic Kid”) have received surgery before they are even a year old. The trend in CI research promotes the idea of lowered age restrictions, with arguments that younger recipients have a better chance of integrating into the hearing society. The issue of ethics is raised because two-third of CI recipients in the United States are children, and they are voiceless in a procedure that requires invasive surgery.[9] Who has the right to the say the deaf need to be fixed is another question of ethics. Inadvertently, the able society has placed a great deal of pressure on those who are different to conform to the norm.
4.1a Prejudice Against the Deaf
Before the invention of cochlear implants, many people of the deaf embraced their identity and viewed deafness as a culture. Advocates of deaf culture aimed to distinguish their status as a culture instead of as pathology. As a culture, the Deaf (with a capital “D”) often experience marginalization from the hearing world due to their deaf (with a small “d”) pathological status.[36] Prejudice and discrimination can pressure those with hearing loss to retreat away from the hearing society, and into the Deaf community for group-inclusion and self-preservation. A strong group identity has strived for many years, but the introduction of cochlear implants has become a concern for Deaf advocates. “Cochlear implants are killing deaf culture,” is a sentimental worry voiced by those in the Deaf community.[37]
Phonocentrism is the belief that spoken language is superior to other modes of communication, such as written or signed language. [38] Photocentrism discriminates against the deaf because auditory impairment hinders the use of oral skills. Sign language, a language commonly used by the deaf community, uses body language to convey meaning and conversation. The lack of audible vocalization from signing is therefore at target for photocentrism.
4.1b Cyborgization
| “What would you do?” |
| "If you could make your deaf children hear, would you do it?" - IMDB. |
Cyborgization is a form of repair or enhancement in a biological organism with an exogenous device. In medicine, implants such as retinal implants, cochlear implants, and auditory brainstem implants (ABI) are considered cyborg-devices. The co-existence of human and machine as a single organism was a science fiction dream in the early 20th century. “Cyborg” was coined in 1960 by Manfred E. Clynes and Nathan S. Kline, when they described the idea of enhancing human beings with the use of machinery.[39] Today a person with a cochlear implant could be thought of as a cybernetic organism. The ethical controversy in cyborgization is that its aim of restoration implies that the human counterpart is damaged, and must be fixed.[38] One must ask if it is fair to view the deaf community as a broken population. Around the world, deaf communities are abundant and immensely proud of their collective identity. American Sign Language, the dominant form of communication among the deaf is legally recognized as an official language that can be used in legal and civil situations.[18]
Peter Artinian of Sound and Fury (2000), an Academy nominated documentary, shared his view on implants and stated, “I’m afraid that cochlear implants will create a bunch of robots.”[37] Artinian’s opinion is contrasted by Michael Chorost, a recipient of a cochlear implant, who wrote the memoir, “Rebuilt: How Becoming Part Computer Made Me More Human." Chorost offers a different view of cyborgization, where machinery has helped him achieve a more “human” life. Implementation of CIs can be thought of as a personal choice, but the ethical ground is particularly shaky when the candidates are children. In 1991, the National Association of the Deaf worried that CIs imposed an “invasive surgery upon defenseless children.” [40] In most cases, parents and guardians of deaf children must decide on the procedure on behalf of their child. Since CIs are most effect in younger patients, potential candidates require the support and consent of their guardians.
The terms cyborgs and cyborgization has arguably acquired negative connotations over the decades from cultured stereotypes. To be a cyborg is perhaps to be less human and more machine. In the medical realm, a cyborg can also be more ambivalently referred to as a bionic human.
4.1c Sound and Fury (2000)
Sound and Fury (2000) is documentary produced by Josh Aronson, which looks into complicated lives of two Artinian families torn apart by conflicting principles. One of hearing and one deaf, the two brothers are fathers in their respected families to a deaf child. Turmoil surfaces when the families must decided whether or not to give their child the surgical procedure to restoring hearing.
In 2005, Aronson returned to the deaf brother and his family to see what had transpired in Sound and Fury 6 Years Later.
This Neurowiki is really interesting! I found a youtube video (http://www.youtube.com/watch?v=LsOo3jzkhYA) that may be helpful in the self-esteem part of your neurowiki. I searched up "cochlear implant hearing for the first time" on youtube, so if this one doesn't suit you, you can always choose an alternative video!
Thanks Timothy! That's a really touching video.
Amazing research. Language acquisition in general is interesting to think about, but I never really thought about the ethical complications of CI before. Really interesting page and layout is well-organized, I'm glad to have read it!
Thanks for the feed back, it's greatly appreciated!